Posttraumatic stress disorder (PTSD) affects untold numbers of people around the world. It has been estimated that upwards of 6% of the U.S. population will experience the condition at least once in their lives. Interestingly, though PTSD has been studied extensively for decades, the severity of its symptoms are still very tough to measure. That makes it tough to treat as well.
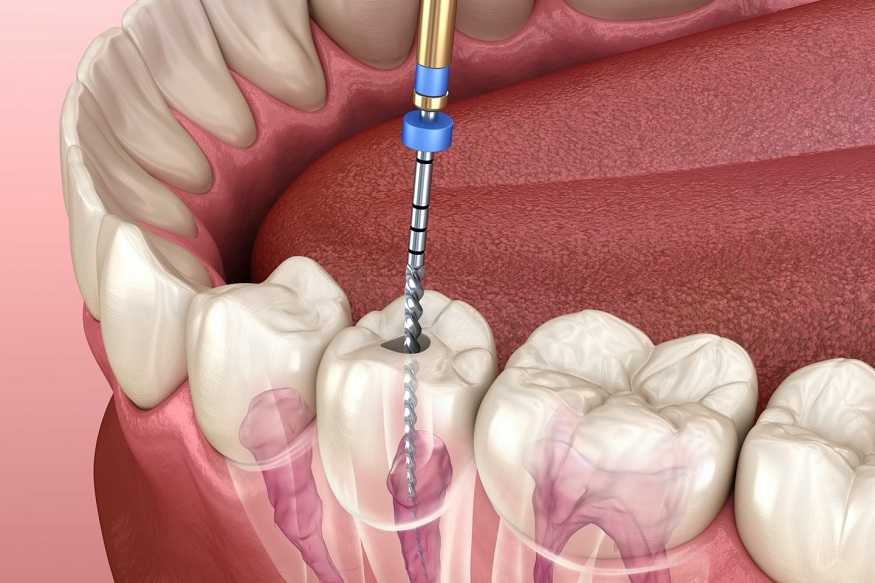
Measuring the severity of a broken bone is pretty straightforward. An X-ray easily reveals in minutes whether a fracture is hairline or complete. A doctor can even see bone fragments and damaged tissue. If only measuring the severity of PTSD symptoms were that simple.
Like chronic pain, PTSD is experienced in a personal way that can be difficult to quantify. Doctors have access to standardized assessment tools but, when all is said and done, symptom severity is determined by a score. Unfortunately, no matter how hard a doctor tries, a score is neither unbiased nor arbitrary.
Two Common Assessment Tools
Determining the severity of a patient’s PTSD symptoms almost always begins with a clinical interview. A doctor or therapist will sit down with the patient to ask targeted questions designed to help them understand the patient’s experiences. Questions related to symptoms and how they impact the patient’s life are the norm. Clinicians often ask questions designed to explore the basic elements of the traumatic event leading to PTSD symptoms.
From there, the clinician will generally rely on a standardized assessment tool. Here are two of the most common tools used today:
- CAPS – The Clinician-Administered PTSD Scale (CAPS) tool is an interview-based tool for assessing the frequency and intensity of the known criteria for PTSD. A CAPS assessment should provide the clinician with a detailed picture of the patient’s symptom experience.
- PTSD Checklist – The PTSD checklist is more or less a survey through which patients self-report their symptoms. Patients are asked to rate each symptom they have experienced and how much that symptom has bothered them. Survey information is used to calculate a severity score.
Both tools can be very helpful in understanding where a patient is with PTSD. But note that they are both subjective. The therapist has one view of PTSD (clinical) while the patient has a very different view (personal experience). Their separate and distinct views undoubtedly impact their perceptions of symptom severity.
Treating the Symptoms
Despite having difficulty determining the true severity of a patient’s symptoms, doctors and therapists still have an obligation to recommend therapies they believe will offer some measure of relief. Traditionally, such therapies have been limited to prescription medications and psychotherapy.
Traditional therapies have worked to some extent. However, not all patients find the necessary relief through the traditional approach. Enter alternative therapies provided through plant-based medicines.
KindlyMD is a Utah medical provider operating multiple clinics throughout the state. They combine Utah Med Card assistance with medication management and psychotherapy to assist PTSD patients who have not found sufficient relief through traditional therapies.
The plant-based medicines KindlyMD practitioners recommend cannot be purchased at chain pharmacies. Patients can’t buy them at the grocery store pharmacy or the neighborhood convenience store. They are only accessible through Utah’s Med Card program.
For some patients, plant-based medicines are effective enough that combining them with traditional therapies offers maximum relief. For others, the plant-based medicines provide the only relief they experience. That is the thing about PTSD. It is very difficult to treat because the symptoms are equally difficult to measure. PTSD patients in some states are fortunate to have access to alternative treatments, like those in Utah.